Travelling with Diabetes; The Challenges Faced & How You Can Overcome Them

It is estimated that 4.9 million people in Britain have been diagnosed with diabetes. Of the 36,000 children that have been diagnosed, 90% of them are also Type 1.
What is Type 1 diabetes?
When the body is no longer able to produce insulin because the insulin producing cells in the body have been destroyed.
What is Type 2 diabetes?
This occurs when the insulin that’s produced in the body doesn’t work correctly, or when insulin producing cells are unable to create enough insulin.
Travelling with Diabetes Medication
As we know, when it comes to hand luggage, security in UK Airports is pretty strict; no liquids over 100ml, restrictions on the size of your bag and of course, no sharp objects!
So what happens when you come to fly but happen to have diabetes for which you may need a high glucose drink or an injection of insulin? Are airports willing to let you take your 150ml can of Coke and your glucose monitor through security without question?
With the help from organisations such as Laborom, Families with Diabetes, DASH and The Leeds Teaching Hospitals NHS Trust we surveyed more than 75 individuals to ask them about their experiences, either personally or those of their children. Whilst some of the answers were astonishing and sometimes rather upsetting, we found a lot of useful information on what airports do well and how they can further help make travelling with diabetes at the airport an easier experience.
What are Airports and Airlines doing already?
The Civil Aviation Authority (CAA) have set out a number of guidelines for both passengers and Airports / Airlines to follow, including contacting your airline before departure to advise them of the equipment and medication that are needed. In some instances, you may be required to fill out additional paperwork before you fly and they highly recommend you bring a letter from your doctor or healthcare professional to authenticate the need for any equipment and insulin. However, as our survey showed, this doesn’t always work…!
On board a flight, most airlines will provide a Diabetic meal – although, this has also received a lot of negative feedback in our survey too! We recommend you do let the airline know about this in advance!
So, what did we find?
To kick off, we’ll start with the question that provoked the most detailed responses: “Have you ever had any issues at Airport Security?”
We found that 55% of the respondents have experienced some form of questioning, “hassle”, confiscation and “rudeness” from Airport security staff, citing that airports in the UK are the biggest culprits.
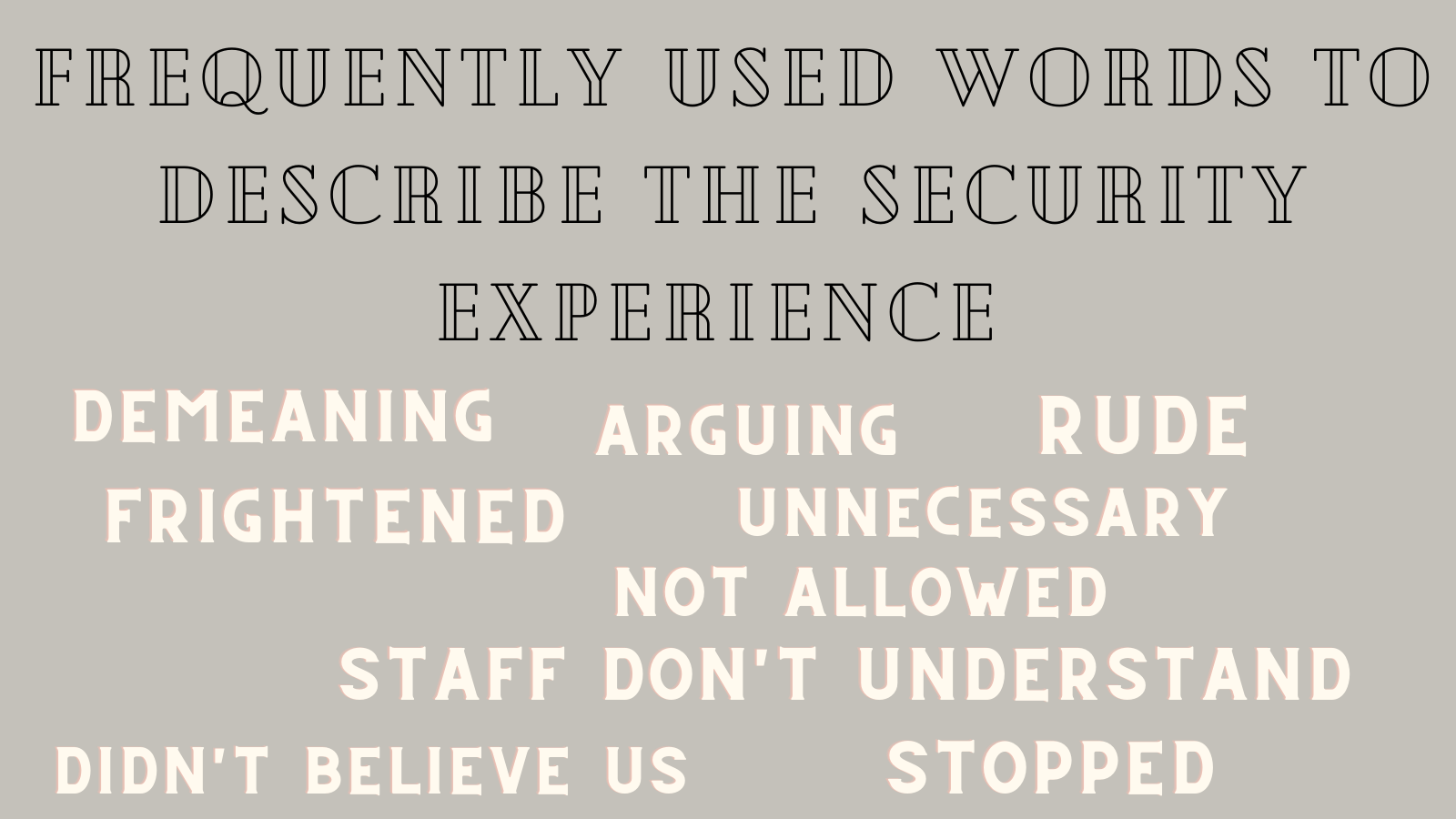
Quite a common response focussed around the lack of understanding of diabetes and what is needed to treat symptoms and prevent hypos. A typical hand luggage bag may contain syringes and of course insulin vials stored in Frio bags as it cannot go in the hold, but what about the bottle of Lucozade and cans of Coke that can also be used as treatment?
Over a third of our respondents discussed having their bottles confiscated and were told to simply buy replacements in duty free. This may sound reasonable, but for some, the actual size of the can or bottle will have the exact amount of glucose needed to treat a hypo. For instance, a 150 ml can of coke may be needed, but not necessarily available to purchase in an airport! One mother told us she and her young daughter had even been marched to a shop to purchase more Lucozade after they had their four 380ml bottles confiscated. When the staff member was happy they couldn’t purchase these in the airport, the confiscated bottles were eventually returned.
Flying with Insulin Pens, Needles and Pumps
Most airlines state when you book that if you expect to be carrying medical equipment, this can be taken free of charge as additional hand luggage – including food, drink and hypodermic needles and syringes. Airlines such as easyJet state that any liquid transported should be under 100 ml BUT if you need to carry in larger quantities, a doctor’s note stating the medicine and quantity should be adequate. So surely this should be the same if a drink is considered “vital” to hypo recovery for some?!
Can I Take My Blood Sugar Monitor On A Plane?
There also seems to be a lot of confusion over the use and transportation of Continuous Glucose Monitors (CGMs) and whether they can be scanned at security and used on aircrafts. In short, a CGM is a small device that uses an electrode placed under the skin to monitor your glucose levels throughout the day, in a bid to prevent a hypo occurring. Most devices are not able to be scanned and a lack of understanding of this on the security staff’s part can lead to frustration, embarrassment and in some cases, crying children.

Here is a quick overview of what the Civil Aviation Authority state about the scanning of devices:
“As there have been some concerns about possible effects of airport security screening equipment on insulin pumps and Continuous Glucose Monitoring systems (CGMs), updated guidance from the Department for Transport is that both insulin pumps and CGMs must not be either screened by x-ray or pass through the security scanner, so will be screened by alternative methods.
If you do not wish to be screened by security scanner you can ask for a hand-search. This may be an enhanced hand-search in private to ensure equivalence with a security scanner. Security staff can exercise discretion as to the extent of the search, subject to the security officer being able to reasonably satisfy themselves that no prohibited article is present.”
If you have a spare medical device in your cabin bag then you should take it out before it goes to the x-ray. You should also let the security officer know about this.
The CAA and Airport Operators Association have helpfully created a Medical Awareness Card for passengers that may be travelling with an insulin pump or CGM. It can remind you about how to prepare for your journey and which documents you should take with you. The card also serves as a reminder for the security officers and lets them know that they should be using alternative security processes.
So, it is unsurprising then to hear that a staggering 71% said they would not feel confident flying alone and potentially relying on staff assistance should they need it. Although a few of our respondents said that they regularly fly solo and hadn’t encountered any issues thus far, most of those with children said that they would not allow their youngsters to fly unaccompanied at all.
What to do if you run out of insulin on holiday?
First and foremost, try to always have spare insulin if You’re travelling with diabetes so can so you can avoid this situation. However, if it does happen, it is more critical for people with type 1 diabetes, where they can go into Diabetic Ketoacidosis within a day. If you have type 2, it’s not as critical but you will start feeling sick.
So what to do until you find some insulin? Here are our recommendations:
- Avoid carbohydrates as this will only make the situation worse!
- Try to find a hospital nearby and let them know that you need insulin because hospitals will always have insulin on hand! However, do bear in mind, it will be costly and quite often, they will only provide you with a day or two’s worth of insulin. So if it’s early on in your trip, it won’t last for the whole holiday. So what you need to do next is try calling or contacting your doctor and see if they can send an email or fax to a local pharmacy store. This way the pharmacy will be able to verify you need the medicine and you’ll have enough insulin for the holiday.
- We recommend printing out your prescription and putting it in a safe place in your suitcase. This way, if this does happen to you, you’ll at least have your prescription at hand and it should save you a lot of stress and panic!

Diabetes in the heat and the cold
Hot climates:
Your worst enemy will be the sun in hotter climates so keep yourself covered! Wear long dresses or long-sleeved T-shirts to protect your skin from the sun. Also, wear a high factor sunscreen such as SPF50. Make sure your sunglasses also have UV400 so your eyes are protected too.
Sunbathing
Whilst sunbathing on the beach is often a priority for most people, it can affect your diabetes as it can make your blood sugar levels higher than usual.
Moreover, your insulin will be absorbed at a much faster rate in hot climates which can then increase your risk of getting hypocalcemia. Therefore, check your levels more frequently and adjust your diet or dose if you have to.
Be wary of getting misleading results as hot weather can affect the accuracy of your meter. Not to mention, if your levels are higher, this may also be because of the weather because heat can cause damage to the insulin which makes it stop working as efficiently.
Storing your insulin in a hot climate
In order to keep it cool, try to store your insulin in a fridge in your hotel room or wherever you may be staying. If there’s no fridge, you can also put it in a cool bag!

Cold climates:
If you’re travelling with diabetes to a cooler place, the opposite will happen. Your insulin will absorb at a much slower rate than normal but will accelerate once you start to warm up. This can again lead to you getting hypocalcemia, especially if your body is shivering to try to stay warm. This can be more dangerous in colder climates because they hinder your body’s attempt to warm up and you can then be at risk of getting hypothermia.
Like hot weather, cold weather can also change the meter reading. So, we recommend warming your hands first, either by rubbing them together or putting them next to a radiator, and then doing the test!
Storing your insulin in a cold climate
Again, in the colder environment, the insulin is at risk of getting frozen. Keep an eye on your insulin and make sure it doesn’t freeze. If you’re going out and worried about it freezing, buy an insulated thermos or cooler. Make sure it stays above 40 degrees if possible! If for any reason, it has frozen, don’t use it, instead use a new one.

Are these problems just in the UK?
We asked if they felt they were treated differently in airports away from home and whether the experience is better or worse abroad.
Unfortunately, the UK came up trumps in terms of bad reviews; Gatwick was described as “difficult” and “always an issue”, Birmingham are “not helpful”, and one respondent had heard such poor reviews of Manchester that they “actively avoid flying” from the airport. Oh dear!
This is in stark contrast to Dublin and Portugal who are “Very good” and “Far more knowledgeable about Type 1”, Turkey who are “amazingly helpful” and The USA where it is “easier to fly from than Gatwick”.
This isn’t all one sided however; Heathrow, Bournemouth and Southampton were all described as helpful and the respondents who mentioned these airports say they have never had any issues travelling with diabetes from them.
In Italy however, the security team noticed that there were less needles in one passenger’s hand luggage than when they entered Italy a week ago. After trying to explain that they had been used, the passenger was questioned and accused of hiding them!
What should Airports and Airlines really be doing?
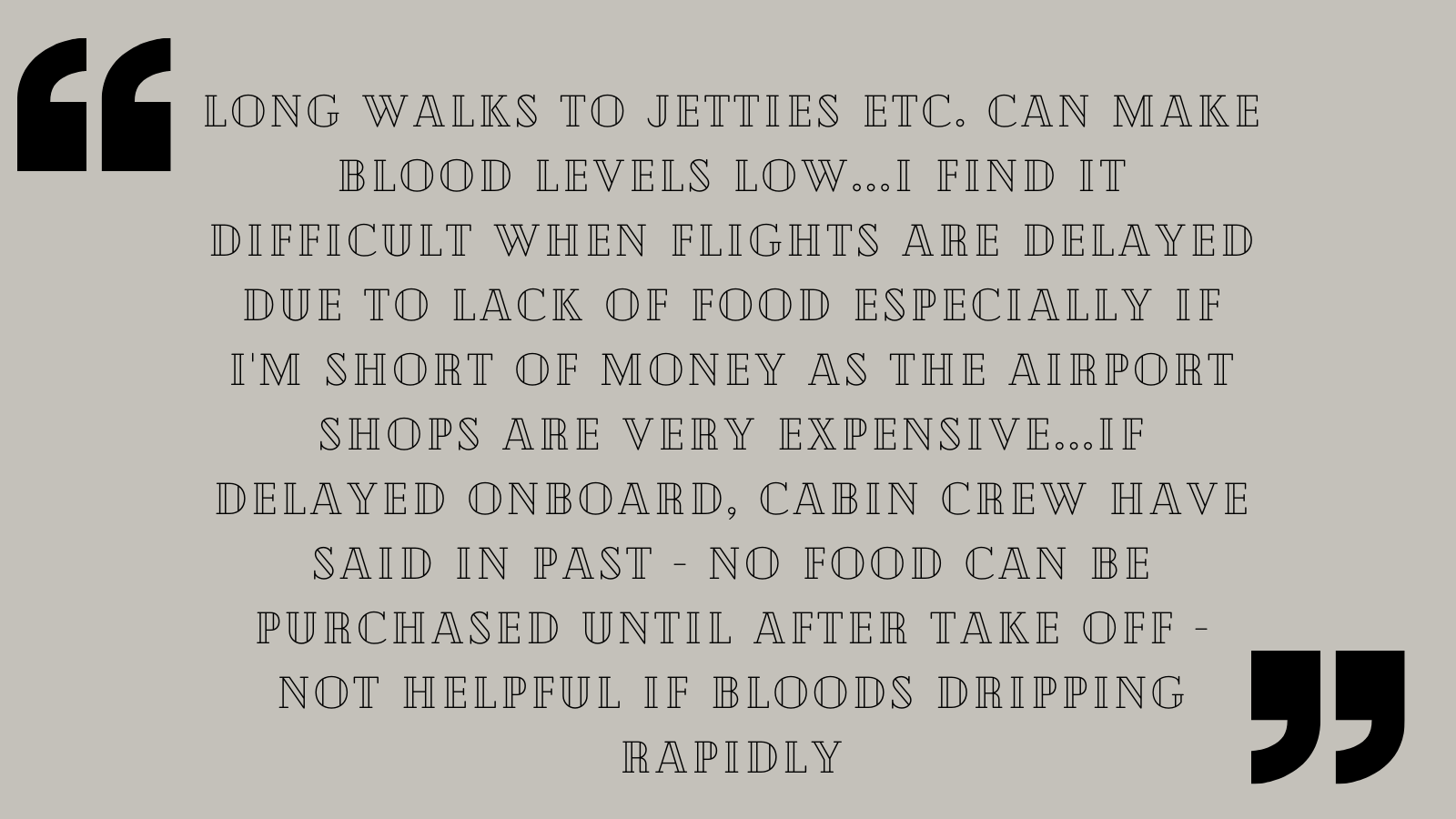
We put the above question to our respondents and there was seemed to be a recurring theme surrounding food, awareness and consistency across the board.
Change Diabetic Meals
These are on offer on many in-flight menus, but in reality, they are low fat and high in carbs; quite the opposite of what is needed to stabilise blood sugars for some people! They always taste bad too, apparently, usually devoid of sauces and generally bland. There’s a recent trend for ‘create your own’ meals on some US airlines to specifically cater for those with a diet controlled condition, and it was suggested many times that this would be appreciated. Many said that they now opt for a regular meal and just eat the parts they are able to!
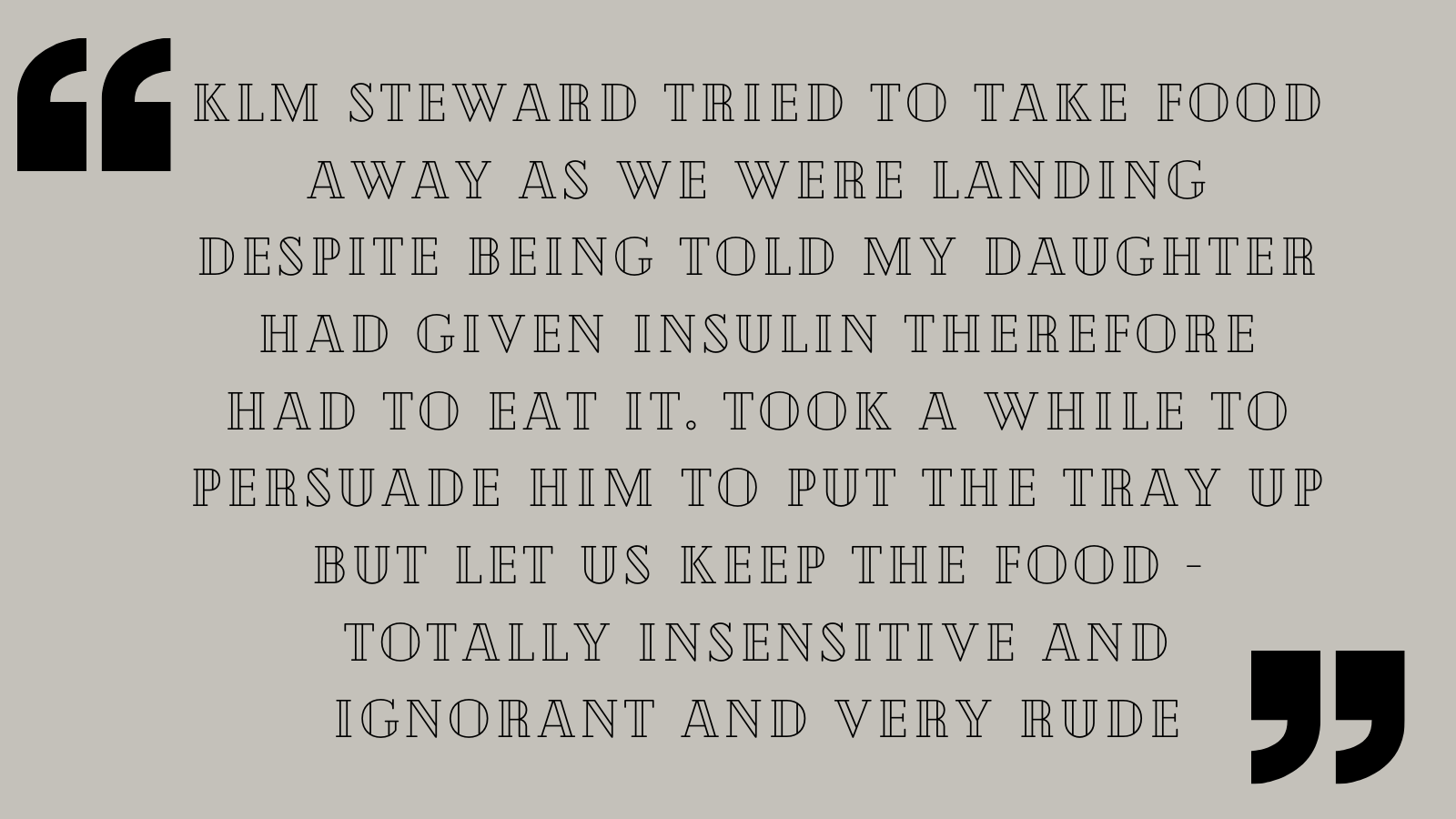
Train the Staff!
Most of the responses mentioned that the lack of training, understanding and knowledge of diabetes by airport staff led to frustration and embarrassment for the passengers. Too many times are people questioned about their CGM’s, and “not believed” when they say their fizzy drinks are for hypos. More so, subjecting children to pat down searches can leave them anxious and confused, sometimes resulting in an eventual hypo brought on by the stress caused by the experience. Even a basic understanding of the difference between Type 1, 2, gestational and Cystic Fibrosis related diabetes would be appreciated, as well as knowing what the CGMs look like and accepting that if a doctor’s note says a sugary drink is used for hypos treatment, they mean it! Going back to the scanner point from the CAA, there should be an understanding across the board that they shouldn’t be scanned to save confusion.
Dedicated Lanes
Although some airline already do this, it was felt that a dedicated “Medical Assistance” lane at airport security would be beneficial, and not just for those with travelling with diabetes. Some of our respondents felt that when they are being scanned for a second time, being made to empty the contents of their bags to match the medical equipment to doctor’s letters and being swabbed, they are holding up other passengers. Most felt this was unfair (to the other passengers) and so a dedicated lane (or two) would be ideal. This could also help with the staff training issues mentioned above – the need for trained staff would be just for those working on these lanes.
Make the rules clear
As we stated earlier, necessary medical equipment can be carried as an extra piece of hand luggage with no extra charge with most airlines, but this isn’t always clear. Our biggest piece of advice would be to call your airport and airline prior to travelling to clarify these details if it isn’t clear on their website or at the time of booking.
We would like to thank all of the organisations we contacted and helped us obtain the valuable feedback, just as much as we’d like to thank everyone that took the time to respond! We really appreciate the time and effort spent on the responses which have helped us write a piece that can hopefully resonate with UK airports. Who knows, we may see changes yet – watch this space!